PROVINCETOWN — In the popular children’s book Stone Soup, the soup is started with no great resources — in fact, it’s just a large pot of water with one stone in it. But as every villager brings something to add — carrots here, potatoes there — the soup grows into something real.
This “everybody brings something” method resembles the approach to asymptomatic testing on Nantucket and at the Community Health Center (CHC) of Cape Cod, which serves the towns of the Upper Cape. In both locations, a variety of actors are contributing resources to make asymptomatic testing a reality. That’s in contrast to the Outer Cape, which has no asymptomatic testing.
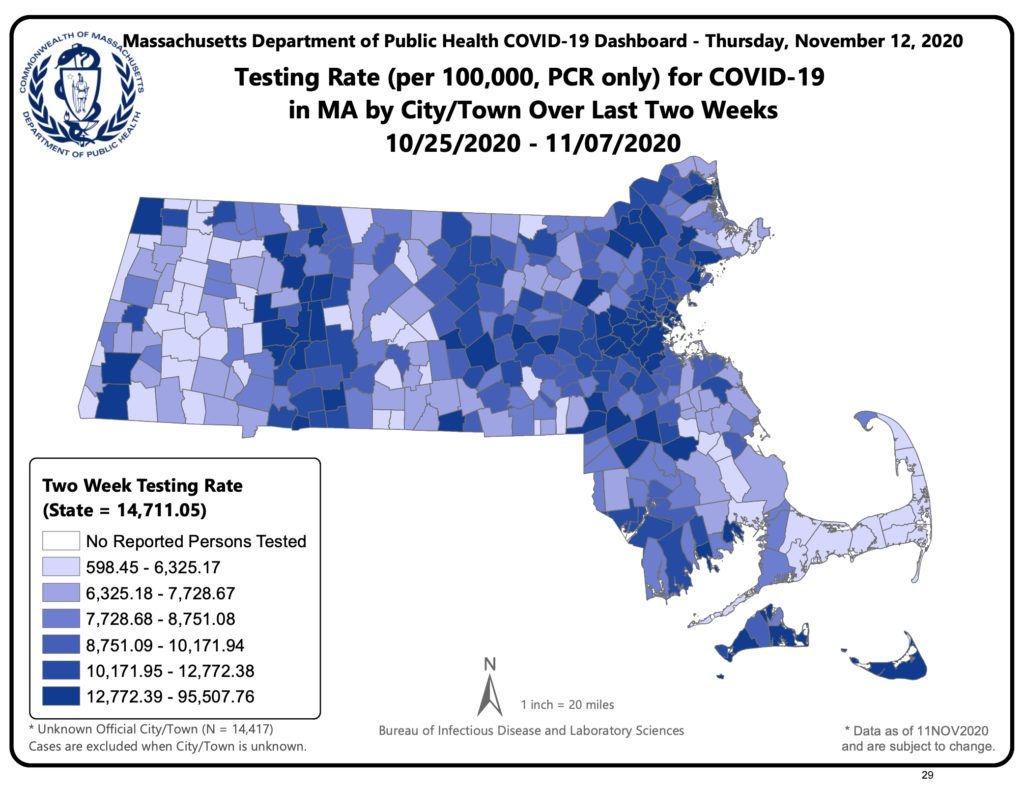
The importance of asymptomatic testing was highlighted by state Sen. Julian Cyr last week, citing a map released by the state.
“The map confirms our suspicions that barriers around appointment times and symptom requirements have resulted in lower testing rates on Cape Cod as compared to the rest of the state,” Cyr said.
“Molecular tests are lower in Barnstable County than its percentage of the statewide population,” he added. “The Mid Cape has an active outbreak, and this is among the lowest testing rates in the state. We are in a dangerous phase, and what we do now is going to determine how dark of a winter we have on Cape Cod.”
To dramatically expand testing involves both rules and resources. The key questions are: Who is eligible for a test? Who will pay for it?
Since the CARES Act passed in March, insurance has been obligated to pay for testing for people with symptoms and people who have been identified by contact tracers as exposed to Covid.
Asymptomatic testing means that people without symptoms or definite exposure are eligible to get tested as well. Once the doors are thrown open to this larger group of people, the question of who pays comes next.
Large-scale testing is expensive. In all of Barnstable County, there have been 116,231 Covid tests performed since March. At $150 per test, that’s $17 million just in this county. The 7 million tests that have been done statewide cost about a billion dollars.
When insurance can’t be billed, the money for expanded testing needs to come from somewhere else.
Everybody Pitch In
Nantucket began its asymptomatic testing program back in June, and it features a hybrid model in which the town pays for certain high-risk workers, individuals pay for themselves, and employers pay for their whole organization. The Nantucket Select Board allocated $100,000 to the program, but only about half that money has been used so far, according to Nantucket’s health director, Roberto Santamaria.
That $50,000 of town money represents roughly 330 tests, or about 10 percent of the asymptomatic program, which is called CastNet.
“We did, for a while, have a lot of employers paying,” said Santamaria. “Some of the landscaping companies had their whole crew tested. The golf club paid to test their entire membership, as well as their employees.”
About 3,300 people had been tested through CastNet by mid-October, when a worsening outbreak caused the state to step in and open a Stop the Spread site on Nantucket. Stop the Spread is a state-financed asymptomatic testing program that is made available to communities with major outbreaks. Between Oct. 15 and Nov. 16, there were 1,841 tests done at the Stop the Spread site on Nantucket, according to Jason Graziadei, information officer at Nantucket Cottage Hospital.
On Nov. 4, the CHC of Cape Cod, which has locations in Bourne, Falmouth, Mashpee, and Centerville, announced that it will begin offering asymptomatic testing as well.
“We’ll be evaluating patients on a case-by-case basis,” said Karen Gardner, CEO of CHC of Cape Cod. “There are people who haven’t been contacted by a tracer, but feel they may have been exposed, maybe through a family gathering, or they hear by word of mouth that a friend of a friend has been exposed. Many times, you can bill insurance, and our triage nurse will go through a series of questions to determine whether it’s clinically appropriate,” said Gardner.
“In other cases — say, someone’s planning to visit a family member, and they just want a test — we wouldn’t bill insurance,” Gardner added. “They either self-pay or we have a sliding scale for incomes under 200 percent of federal poverty level.” Two hundred percent of the FPL is $25,500 per year for a single person, or $52,400 for a family of four.
Self-payment would be around $150, said Gardner, which covers the specimen collection and the laboratory fee. “We’re not charging it as a doctor visit,” said Gardner.
CHC of Cape Cod received a donation from Martha’s Vineyard Savings Bank, which helped underwrite the scheduling software behind the asymptomatic program. “It takes a tremendous amount of I.T. interface and data entry work, and the grant, in part, is funding that,” said Gardner.
“We were doing about 100 tests a week, right before we opened it up” to asymptomatic people, Gardner added. “At the end of last week, our staff said our phone calls had doubled and we had basically doubled our capacity. If we have much growth beyond that, we’ll need to expand our testing hours and have a dedicated testing team. We have the physical capacity — it’s just a matter of restructuring staffing to meet the demand.”
Why Not Here?
Right now, Outer Cape Health Services tests only symptomatic and contact-traced people. The nearest site for asymptomatic testing is CareWell Urgent Care in Dennis.
For many months, there were essentially no Covid cases on the Outer Cape. Provincetown’s health dept. ran three separate asymptomatic testing events, timed to follow high-traffic weekends in the summer and fall. Health Director Morgan Clark couldn’t be specific about the results of those tests, but case reports from those months show a long string of zero cases in Provincetown. Wellfleet and Truro showed a string of zeros as well.
Now, however, the data are changing rapidly. There were four cases in Provincetown at the end of October. There are four cases in Wellfleet this week. Fall River, New Bedford, Rhode Island, and Nantucket have an explosion of cases.
“I worry that we do not have the testing capacity that we need here,” said Cyr. “We’re going to continue to work on this. We need more testing resources if we are going to meet the challenges of this moment.”

