PROVINCETOWN — The official case counts for monkeypox are still low — 13 cases in Massachusetts, 63 in New York as of Tuesday, June 28. But the numbers have been doubling about every seven days, and public health leaders want the public to know how the disease spreads, what the symptoms are, and what kind of care is available to people who catch or are potentially exposed to it.
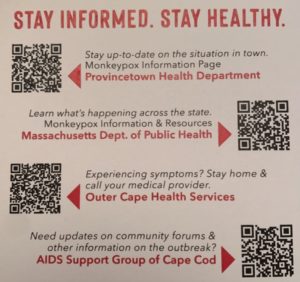
At a community forum on Tuesday, officials of the state Dept. of Public Health joined government and nonprofit leaders from across Cape Cod to answer questions about monkeypox and the state’s medical response.
Monkeypox is not a new disease. Multiple strains have been endemic in central Africa since at least the 1970s, said Kevin Cranston, assistant commissioner of the DPH. The virus is related to smallpox, and vaccines for smallpox have proven effective against monkeypox.
The multinational outbreak that is happening in Europe and the Americas has primarily affected gay and bisexual men and men who have sex with men (MSM) but don’t identify as gay. According to the World Health Organization, “most but not all” of the cases that have appeared outside of Africa in May and June this year — 4,700 or so cases in all — have been in the gay or MSM population.
That is because of the virus’s initial appearance at “events that were identified in Europe” — the British and American press have identified a week-long gay pride celebration in the Canary Islands in early May — and the virus’s tendency to spread along lines of extremely close skin-to-skin contact, said Cranston.
“Gay men may be the ecosystem that the virus is taking advantage of at this time, but it’s not limited to them by any means,” said Cranston, who identified himself as gay at the outset of the forum.
Key variables distinguish the current monkeypox outbreak from Covid or other epidemics, Cranston added. The method of spread, the time to contagiousness, and the existence of treatments and vaccines are all important differences.
“While we are anticipating this will be an ongoing outbreak, we don’t consider this a pandemic-level event,” said Cranston. “This is not a respiratory virus. This is not a virus that is easily transmitted. It requires extremely close skin-to-skin contact between a symptomatic infected individual and an uninfected individual.”
Other forms of transmission do exist, but they typically involve people who are living with or providing care to people with visible illness. “Respiratory contact — we are talking extended, close, almost face-to-face, for six hours or more,” said Cranston.
“There’s no general recommendation for handling laundry in a different way,” said state epidemiologist Catherine Brown. “If I were talking to people working in the service industry, I could imagine wearing gloves and not shaking the linens out vigorously before laundering, but standard laundry practices are sufficient.”
In other words, both respiratory and laundry-based transmission are seen as problems faced by the partners, roommates, and caretakers of people who are conspicuously ill — not as avenues of stealth transmission or spread.
“There is no evidence the virus is transmitted before a person is symptomatic,” Cranston added. “That’s good news.”
Symptoms typically begin with a flu-like cluster: headache, body aches, malaise, fever, chills, and swollen lymph nodes. Not long after come a variety of skin manifestations, including “a flat rash, raised macules, the actual pox, which often has a little navel in the center of it, and vesicles of fluid under the skin, and pockets of fluid emerging through the skin,” said Cranston.
The “skin manifestations” and fluids are especially contagious, but transmission is possible from the appearance of the first symptoms until the last scab has fallen off — often around four weeks in all.
No one has died of monkeypox during this outbreak — but the infection is painful, and it can leave scars. No one has been hospitalized for lifesaving care either, but there have been some hospitalizations for pain management, Dr. Brown said.
There is an unusually long latency period between exposure and the development of symptoms — 6 to 21 days. A vaccine called Jynneos, which is made from a related virus that can no longer replicate, can be given to people who have been exposed to monkeypox and haven’t yet developed symptoms. It prevents them from getting the disease.
Having time to identify contacts and prevent transmission of the virus is something like the Holy Grail in public health. DPH leaders and state Sen. Julian Cyr, who moderated the forum, said that getting access to more Jynneos vaccine is the most pressing conversation.
“At this point, the vaccine is primarily being used post-exposure for high-risk close contacts,” said Brown. “We are working to make sure we get that vaccine to those contacts as promptly as possible. There’s a lot of interest in what role pre-exposure vaccination can play. The feds are talking about it, but we have to be realistic about the amount of Jynneos vaccine they currently have. They’re working with the manufacturer to speed up supply and are expecting additional doses in July and then more through this year. But the feds are the sole supplier of Jynneos right now.”
There have been around 30,000 courses of Jynneos vaccine (a course is two doses, four weeks apart) distributed to the states thus far, said Dr. Larry Madoff, medical director of the state’s Bureau of Infectious Disease. Massachusetts has received “hundreds, not thousands” of doses, Cyr said. More are expected soon — in fact, at the Independent’s deadline, the federal government released another 56,000 doses to the states. In the near term, the focus is likely to remain on vaccinating the contacts of people who develop symptoms.
Given current supplies, “We need clear evidence of contact — not more distal contact,” said Cranston. Sharing a bed would definitely qualify; sharing a dance floor probably would not.
“The number of cases we’re dealing with and the transmission dynamics of this virus do not say that people should stop going to parties and stop dancing,” said Cranston. “An individual may say, ‘I may not want to have the skin-to-skin contact I would normally have on a night I go out,’ ” he added, but current facts are not leading public health authorities to target dance floors.
Nonetheless, one doesn’t have to wait for a contact tracer to call, either.
“If someone has good evidence of exposure to someone with monkeypox, and they believe they’re eligible for post-exposure, they need to go to their care provider and their provider will reach out to us,” said Brown.