PROVINCETOWN — When it comes to Covid, Massachusetts is pro-data. The Dept. of Public Health (DPH) publishes a weekly Covid report, daily Covid updates, and a weekly report on vaccinations. Case rates and death rates for individual nursing homes have been published every week since May, as well as other data, such as staff testing rates and infection control surveys.
But when it comes to assisted living, information is not that forthcoming. Covid reports don’t identify death rates for residents in assisted living facilities, even though they’re one of the most vulnerable populations in the state.
Partly, this has to do with legal differences. Nursing homes, or long-term care facilities, are treated like hospitals and regulated by the DPH. Assisted living facilities are a housing arrangement with medical support, and are thus regulated by the Executive Office of Elder Affairs (EOEA).
Medical privacy laws are also a factor, and, since the pandemic began, family visitation to elder-care facilities has been dramatically curtailed. This has made information about conditions in assisted living facilities difficult to assess. Covid fatality reports are one of the few kinds of data that can be requested from state regulators.
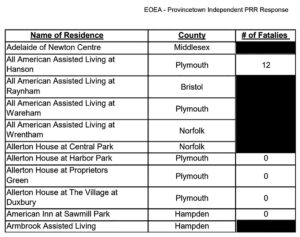
The Independent asked the elder affairs office for three reports on Covid deaths in the state’s 267 assisted living facilities — for the springtime wave (March 1 through May 31), the summertime lull (June 1 to Sept. 30), and the winter wave (Oct. 1 to Jan. 14).
The goal was to find out if Covid protocols instituted in the spring were keeping residents safe through the summer and into the winter wave that swelled in November and December.
But the reports that were delivered are so heavily redacted it’s hard to discern patterns.
It’s widely known that the beginning of the pandemic was horrific in elder-care facilities. By the time the lockdown was enforced, Covid had already spread to nursing homes and other kinds of elder housing across New England. Death numbers were staggering. To this day, more than half of all of the state’s Covid deaths are among nursing home residents.
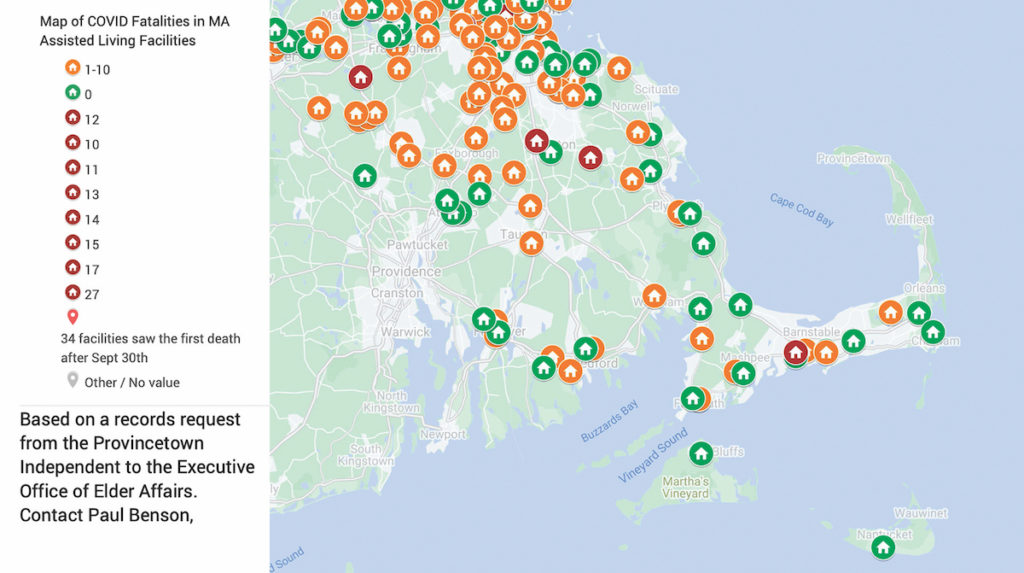
The new data on assisted living facilities line up with that story. Almost half of all assisted living facilities in the state experienced Covid fatalities last spring.
But because of the redactions, a full tally of those deaths can’t be made. (The Independent has put in a request to the EOEA for the total number of spring fatalities; when it is provided, this story will be updated online.) Even so, it’s still possible to see that, of the 143 facilities that had no deaths in the spring, only two went on to see their first deaths in the summer. The protocols on personal protective equipment, social distancing, visitation, and staffing that the industry and regulators put in place helped prevent the spread of Covid, at least in the summer, when the case counts in the Northeast were low.
Between Oct. 1 and Jan. 14, however, 34 assisted living facilities that had previously not seen deaths from Covid saw their first deaths. One of them, Atria Marland Place, in Andover, saw 14 people die during that period.
In Barnstable County, the Mill Hill Residences, in Yarmouth; Atria Woodbriar Park, in Falmouth; and Bridges by Epoch, in Mashpee, had no deaths from Covid as of Oct. 1, yet all have seen from 1 to 10 people die of Covid since then.
Five other Barnstable County facilities have seen deaths from Covid, all of them beginning in the spring wave: Cape Cod Senior Residences at Pocasset, in Bourne; Atria Woodbriar Place, in Falmouth; Brookdale Cape Cod, in Barnstable; Maplewood, in Brewster; and Harbor Point, in Centerville. All of them had between 1 and 10 deaths as of Jan. 14, except Harbor Point, which had 12.
The unspecified range of 1 to 10 deaths is due to the EOEA’s redaction protocol: all numbers from 1 to 10 are obscured. Only eight facilities in the state crossed beyond 10 deaths and were unredacted. That means the most significant information that can be gleaned from the documents is the point at which facilities had more than zero deaths. (The highest tally was 27 deaths, in the Falls at Cordingly Dam, in Newton, all before May 31.)
The EOEA cites the Center for Medicare and Medicaid Services and the Health Insurance Portability and Accountability Act (HIPAA) as its guidelines for redactions. The state DPH interprets those laws differently, and suppresses only numbers between 1 and 4. That, combined with weekly reporting of numbers, is why the situation at nursing homes is so much clearer than it is with assisted living.
The state does publish a “Chapter 93 Elder Facilities Daily Report,” but that information is self-reported by the facilities and is filled with errors and omissions. For example, of the nine Atria assisted living facilities, only three had any deaths in the Chapter 93 report, yet the redacted state documents show that there were deaths in eight out of nine of them.
Similarly, of the five Benchmark properties in the state’s listing, there were Covid deaths in all five. The Chapter 93 report shows deaths in only two.
There’s no geographic pattern to the deaths. The statewide map shows that the losses aren’t concentrated anywhere. But when it comes to elder care, pain and loss is pretty much everywhere.