
PROVINCETOWN — In a recent press call, state Sen. Julian Cyr sounded an alarm about coronavirus testing on Cape Cod.
“We see the cases coming south and east towards Cape Cod,” said Cyr. “We have an opportunity to get ahead of this. Gov. Baker’s administration hasn’t released $550,000 in funding to Barnstable County for testing. My patience is wearing thin on the failure to release this money.
“These are resources that state Sen. Moran and state Rep. Fernandes secured in the legislature,” Cyr continued, “specifically for Covid testing to be coordinated by the Barnstable County Dept. of Health. We want expanded asymptomatic testing. We want these resources released.”
Allowing those without symptoms to be tested has become an issue because the number of Covid infections is rising dramatically in mainland Massachusetts. Given the nature of human transmission, health officials expect cases will travel here as well.
Indeed, four cases were reported in Provincetown in the last days of October, and contact tracers established that all four were related to travel, according to Provincetown Health Director Morgan Clark.
Asymptomatic testing is important early in an outbreak. Because so many people can have few or no symptoms, an outbreak can be well on its way before people start showing up sick at clinics. Catching infections through asymptomatic screening can find cases early enough that contact tracing and isolation orders are still very effective.
The catch, of course, is that testing large numbers of healthy people isn’t cheap. And if it’s overdone, it can gum up the labs that process tests and delay everyone’s results. Even when testing is kept well in line with lab capacity, the costs can add up quickly. Martha’s Vineyard seems to have found a way around this, however, by doing something bold: billing the insurance companies.
How to Handle Costs
The simplest approach to minimizing costs is emphasizing what insurance definitely will pay for — that’s testing for people with symptoms, and testing identified close contacts of those who have tested positive. The list of symptoms is quite long, and includes things like headache and fatigue. Who isn’t a little tired these days?
But frontline workers are specifically instructed not to work if they feel any symptoms at all. It can be hard to coax them into a test.
Both Provincetown and Nantucket have targeted frontline workers with free testing sites that are explicitly for asymptomatic people. Provincetown ran one such event on July 22, timed to follow the busy Fourth of July weekend.
Nantucket has had a rolling invitation to various groups of frontline workers — including home health aides, grocery workers, clergy, and transportation workers. Provincetown spent $15,000 on the July 22 event, while the Nantucket Select Board allocated $100,000 to its testing-by-invitation program.
At an industry-standard $150 a test, though, $100,000 would cover only 667 tests. Even at scale, and with labor costs trimmed by using volunteers where possible, Cyr said the per-test cost is between $80 and $140. At the lower number, $80, Nantucket’s $100,000 would fully cover 1,250 asymptomatic tests.
That sounds like a lot, until you look at the scale of some testing efforts. Nantucket has done 12,000 tests in all since the pandemic started. Martha’s Vineyard has done a total of 26,000.
Make Insurance Pay
Three-quarters of the tests done on the Vineyard have been at a drive-through, anyone-can-come testing site for asymptomatic people. It relies on a mix of staff and volunteers to help lower costs, but 19,500 asymptomatic tests is still a lot of money.
The Vineyard is relying on a mix of strategies to make this test center work, but one of the key ones is just billing health insurance companies.
“We think there’s a gray area here, and it can be captured in two words — medically necessary,” said Cynthia Mitchell, CEO of Island Health Care. “We have chosen to interpret ‘medically necessary’ very broadly: it’s to protect people from getting Covid.”
“Whether we’ll get the reimbursements we’re due across the board remains to be seen, but we are billing, and we’re getting a fair amount of revenue in,” Mitchell added.
“This is a drive-through, so we’re billing for the specimen collection, and that’s all we’re billing,” Mitchell continued. Quest has not been donating the processing fees.
“Quest Diagnostics bills the insurer for processing the sample,” said Mitchell.
Mitchell said Island Health has had great support from Quest staff — Quest’s CEO is a seasonal resident of the Vineyard — who helped set them up with an online registration system for setting up appointments. This has been important, she said. “But it was actually our revenue cycle contractor that worked with us to get the insurance coding right, so the reimbursements would come,” she added.
Mitchell isn’t aware of another community health center using this approach. “It was ambitious,” she said.
The program also benefited from early support from Martha’s Vineyard Bank, which donated $100,000 to help cover testing for the uninsured. And seven Island families gave $150,000 in July to help staff the new online registration system.
Mitchell also cited the CARES Act. “Every health center in the country received $500,000 as a base, and then there was a per-patient number tacked on,” she said. “Because we’re so small, the benefit of that $500,000 was wonderfully disproportionate.”
When to Test
“Who pays?” isn’t the only riddle to solve, though — when to test is important too.
It’s possible to spend a lot of money to consistently find no cases. A long string of zeroes is a relief, of course, but it can also feel like a waste of resources — until suddenly it’s not.
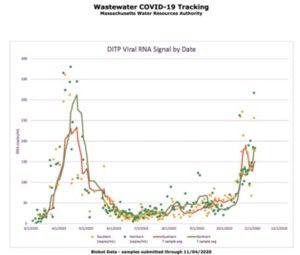
mwra.com/biobot/biobotdata.htm
Martha’s Vineyard had a very low case rate for a long time. Now, however, the asymptomatic testing program has found 47 infections, and, according to Mitchell, some of the other 96 cases on the island were discovered because they’re contacts of those 47. Detecting that outbreak early has allowed for effective contact tracing, said Mitchell.
“I worry that we relied on green / yellow / red to allocate testing resources,” said Cyr. Barnstable County had few cases, in other words, and now it’s doing little testing, leaving it exposed as the statewide situation grows worse.
One possible solution involves testing wastewater for evidence of RNA from SARS-CoV-2, the virus that causes Covid-19. There’s no evidence that people can get sick with Covid from wastewater, but testing it can provide an indication of when large-scale screening should be deployed.
A review of wastewater test results on Nantucket showed that the data tends to be “noisy” — but there were three significant spikes in the numbers, and they were each followed by a wave of newly discovered cases. Wastewater testing isn’t widely used yet, but if it can tell us when to roll out large-scale testing programs, it could help solve the when-to-spend puzzle.



